Systemic lupus erythematosus is a systemic autoimmune disease (or autoimmune connective tissue disease) that can affect any part of the body. As occurs in other autoimmune diseases, the immune system attacks the body's cells and tissue, resulting in inflammation and tissue damage. It is a Type III hypersensitivity reaction in which antibody-immune complexes precipitate and cause a further immune response.
SLE most often harms the heart, joints, skin, lungs, blood vessels, liver, kidneys, and nervous system. The course of the disease is unpredictable, with periods of illness (calledflares) alternating with remissions. The disease occurs nine times more often in women than in men, especially in women in child-bearing years ages 15 to 35, and is also more common in those of non-European descent.
There is no cure for SLE. It is treated with immunosuppression, mainly with cyclophosphamide, corticosteroids and other immunosuppressants. SLE can be fatal.
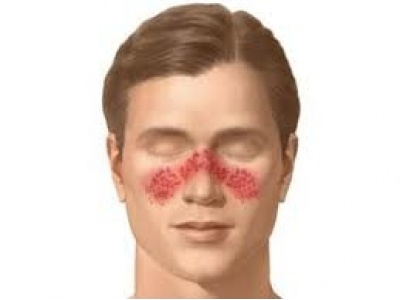
Childhood systemic lupus erythematosus generally presents between the ages of 3 and 15, with girls outnumbering boys 4:1, and typical skin manifestations being butterfly eruption on the face and photosensitivity.
Signs and symptoms
Common initial and chronic complaints include fever, malaise, joint pains, myalgias, fatigue, and temporary loss of cognitive abilities. Because they are so often seen with other diseases, these signs and symptoms are not part of the diagnostic criteria for SLE. When occurring in conjunction with other signs and symptoms (see below), however, they are considered suggestive.
There is no one specific cause of SLE. There are, however, a number of environmental triggers and a number of genetic susceptibilities.
Laboratory tests
Antinuclear antibody (ANA) testing and anti-extractable nuclear antigen (anti-ENA) form the mainstay of serologic testing for SLE. Several techniques are used to detect ANAs. Clinically the most widely used method is indirect immunofluorescence (IF). The pattern of fluorescence suggests the type of antibody present in the patient's serum. Direct immunofluorescence can detect deposits of immunoglobulins and complement proteins in the patient's skin. When skin not exposed to the sun is tested, a positive direct IF (the so-called Lupus band test) is an evidence of systemic lupus erythematosus.
ANA screening yields positive results in many connective tissue disorders and other autoimmune diseases, and may occur in normal individuals. Subtypes of antinuclear antibodies include anti-Smith and anti-double stranded DNA (dsDNA) antibodies (which are linked to SLE) and anti-histone antibodies (which are linked to drug-induced lupus). Anti-dsDNA antibodies are highly specific for SLE; they are present in 70% of cases, whereas they appear in only 0.5% of people without SLE.The anti-dsDNA antibody titers also tend to reflect disease activity, although not in all cases. Other ANA that may occur in SLE sufferers are anti-U1 RNP (which also appears in systemic sclerosis), SS-A (or anti-Ro) and SS-B (or anti-La; both of which are more common in Sjögren's syndrome). SS-A and SS-B confer a specific risk for heart conduction block in neonatal lupus.
Other tests routinely performed in suspected SLE are complement system levels (low levels suggest consumption by the immune system), electrolytes and renal function (disturbed if the kidney is involved), liver enzymes, and complete blood count.
The lupus erythematosus (LE) cell test was commonly used for diagnosis, but it is no longer used because the LE cells are only found in 50–75% of SLE cases, and they are also found in some people with rheumatoid arthritis, scleroderma, and drug sensitivities. Because of this, the LE cell test is now performed only rarely and is mostly of historical significance.
Prevention
SLE cannot be prevented, but the consequences can be prevented.
As longevity of people with SLE increases, the likelihood of complications also increases in four areas: cardiovascular disease, infections, osteoporosis, and cancer. Standard preventive measures, screening for related diseases may be necessary to deal with the increased risks due to the side effects of medications. Extra vigilance is considered warranted in particular for cancers affecting the immune system.
Treatment
The treatment of SLE involves preventing flares and reducing their severity and duration when they occur.
Treatment can include corticosteroids and anti-malarial drugs. Certain types of lupus nephritis such as diffuse proliferative glomerulonephritis require bouts of cytotoxic drugs. These drugs include cyclophosphamide and mycophenolate.
Hydroxychloroquine (HCQ) was approved by the FDA for lupus in 1955. Some drugs approved for other diseases are used for SLE 'off-label'. In November 2010, an FDA advisory panel recommended approving belimumab (Benlysta) as a treatment for the pain and flare-ups common in lupus. The drug was approved by the FDA in March 2011.N-acetylcysteine has been shown to reverse depletion of the natural anti-oxidant glutathione and to safely improve disease activity in a double-blind placebo-controlled pilot study.

